5 May 2025
A Guide to Digital Health Records at Hospitals
“Did you know that nearly all hospitals have adopted electronic health records (EHRs)? According to the National Institutes of Health (NIH), EHRs are digital versions of patients' paper charts, designed to provide real-time, secure access to vital health information.”
These systems revolutionise how medical information is stored and shared, enhancing healthcare delivery efficiency, safety, and speed. But what do digital health records mean for you as a therapist? Let's explore how digital health records are reshaping the future of healthcare. First, let's simply understand digital health records.
What are Digital Health Records?
Imagine having instant access to everything you need to make informed decisions about a patient’s care—no need for repeated history-taking, unnecessary delays, or guesswork. That’s the advantage of digital health records.
These powerful tools enable better, more precise care by putting a patient’s complete medical history at the patient's fingertips. Whether fully digital or a hybrid system of paper and electronic records, the objective remains the same:
- Better clinical decisions: Access accurate, real-time information when it matters most.
- Streamlined processes: Reduce redundant paperwork and avoid repeating unnecessary tests.
- Fewer errors: Centralised records minimise mistakes and improve coordination across teams.
This means faster, safer, and smarter care delivery whenever needed for healthcare professionals. Digital health records are the backbone of modern hospitals, designed to support you in putting patient health first.
Now that you know about digital health records, let’s explore their key components and see how they enhance patients' medical care.
Components of Digital Health Records
Digital health records are more than just files stored on a computer. They’re designed to give you and the patient's healthcare provider a clear, organised view of the patient's medical information, all in one place. Let’s break down the key components of these records to show how they make patient care better and more efficient.
1. Basic Information at a Glance
A patient's digital health record starts with the essentials: The patient's name, age, and contact information. But it goes beyond that. It includes details like why they visited the hospital, what symptoms they reported, and the findings from the patient's examination.
2. Clear Documentation of Patient Care
Every critical aspect of the patient's care is carefully documented. From the results of tests and key examination findings to the treatment plan the therapist has outlined, it’s all there. The patient's digital record also includes information about any medications prescribed and notes about any follow-ups or instructions you’ve been given.
3. Communication Notes
Sometimes, the little details matter the most. Digital health records also store notes from conversations with your therapist or care team. These could include discussions about patients' concerns, any questions they may have asked, or updates on how they respond to treatment.
4. Real-Life Impact
Think about how much time and stress this system can save. For instance, if a patient is travelling and needs medical care, the patient's digital health record allows therapists to instantly see the patient's history, from allergies to past treatments. This can prevent serious errors, like prescribing a medication to which the patient is allergic.
Imagine you are managing a chronic condition. Your therapist can easily track changes in your test results over time, adjust your treatment plan, and coordinate with specialists—all without needing to repeat your medical history. This seamless care isn’t just convenient; it can be life-saving.
Importance of Accurate Digital Documentation
Accurate digital documentation isn’t just about keeping neat records—it’s the backbone of effective healthcare. When a patient's medical history is recorded correctly, it creates a reliable and complete picture of the patient's health, which benefits you in ways you might not even realise.
1. Reflecting on Clinical Events and Decisions
Every note in the patient's digital health record tells a story about the patient's care. From the symptoms you report to the treatment plans the therapist chooses, these records capture the clinical events and decisions that guide the patient's care. This level of accuracy is vital for the therapist to track the patient's progress and make informed decisions about the patient's future treatment.
For example, if a patient is managing a long-term condition like high blood pressure, the patient's record will show how the condition has changed over time, which medications worked best, and what adjustments were made. This helps ensure that every patient care decision is grounded in accurate, up-to-date information.
2. Ensuring Continuity of Care and Accurate Coding
When a patient's care involves multiple healthcare providers, accurate documentation ensures everyone is on the same page. Whether the patient is seeing a specialist, getting a second opinion, or transitioning to a new therapist, the patient's digital health record provides a seamless handoff. This means you don’t have to repeatedly explain the patient's history or worry about missing key details.
Accurate documentation also plays a crucial role in medical coding and billing. It ensures that procedures, diagnoses, and treatments are correctly coded, reducing errors and ensuring patients' insurance claims are processed smoothly. For you, this means fewer headaches with paperwork and more focus on the patient's health.
Now that we have seen the significance of accurate digital documentation, let’s explore its key benefits and challenges.
Benefits and Challenges of Digital Health Records
Digital health records have transformed patient information management, providing significant benefits while introducing specific challenges. Here’s a breakdown tailored for healthcare professionals.
Key Benefits
- Streamlined Information SharingDigital records enable the seamless sharing of patient data across departments and facilities. This reduces redundancies, ensures timely access to critical information, and improves care coordination.
- Enhanced patient SafetyComprehensive documentation minimises errors, such as prescribing conflicting medications or overlooking allergies. Accurate records also improve diagnostic precision and treatment outcomes.
- Accountability and ComplianceTime-stamped and securely stored entries create a transparent record, protecting providers and institutions from medico-legal risks. This traceability ensures adherence to regulatory and ethical standards.
Challenges that you come across
- Dependence on Accurate DocumentationIncomplete or inaccurate data entry can compromise patient safety, leading to misdiagnoses or inappropriate treatments. Therefore, it is critical to maintain thorough and error-free documentation.
- Interoperability IssuesIncompatibilities between systems can hinder the sharing of patient information across facilities, undermining the primary goal of digital health records. Addressing system integration remains a key challenge.
- Data Privacy and Security ConcernsUnauthorised access or data breaches can expose sensitive patient information, leading to privacy violations. Therefore, it is crucial to ensure robust security measures to protect data.
- Clinical Workflow DisruptionsNew digital health technologies can disrupt workflows, leading to inefficiencies or clinician burnout. Practical training and support are necessary to mitigate these disruptions.
While digital health records offer numerous benefits, effectively maintaining them is key to maximising their potential and ensuring their reliability and security.
Guidelines for Maintaining Digital Health Records
Digital health records play a critical role in modern healthcare, and maintaining them properly ensures they remain accurate, secure, and valuable. By following essential guidelines, healthcare providers can improve care quality and patient trust while meeting legal requirements.
1. Ensure Clarity and Objectivity
Clear and precise documentation is vital to avoid misunderstandings affecting patient care.
- Avoid abbreviations: For example, instead of writing “HTN,” document “hypertension” to eliminate ambiguity.
- Be specific. Use objective language, such as “patient reports a headache for two days,” rather than vague terms, such as “unwell.”
- Ensure legibility: While digital records minimise handwriting issues, clear and consistent formatting makes information easier to interpret.
2. Protect Confidentiality
Safeguarding patient data is non-negotiable in maintaining trust and compliance with regulations.
- Access controls: Only authorised personnel should access patient records.
- Secure storage: Use encrypted systems to store health records safely.
- Patient privacy: When discussing sensitive conditions like mental health or chronic illnesses, ensure the information is shared only with those directly involved in the patient’s care.
- Audit Trails: Maintain logs of who accessed patient records and when to ensure accountability and traceability.
- Data Minimisation: Only the essential information necessary for patient care is collected and stored to reduce the exposure risk and ensure compliance with privacy regulations.
With these foundational practices, let’s explore how legal and national guidelines ensure uniformity and reliability in digital health records worldwide.
Legal and National Guidelines
Legal frameworks and national standards set the foundation for managing digital health records across healthcare systems.
1 .Country-Specific Standards
Regulations vary globally, but the focus remains the same: ensuring accurate, secure documentation.
- Example: The Australian Privacy Act 1988 is critical in safeguarding patient data, emphasising protecting personal health information and the right to privacy. This law outlines clear guidelines for collecting, storing, and sharing health records, ensuring that patient data is kept secure and used responsibly.
The EU’s General Data Protection Regulation (GDPR) also prioritises patient data protection, with specific provisions for the right to access and control personal health records. It focuses on empowering individuals with the right to know how their data is used and to have it erased upon request.
Similarly, in the U.S., HIPAA (Health Insurance Portability and Accountability Act) laws focus on securing health information, ensuring that patient data remains confidential, and facilitating the portability of records across healthcare providers.
- Interoperability priorities: In some countries, such as Australia, healthcare systems are designed to allow seamless data sharing between hospitals and clinics for continuity of care.
2 .Professional Guidelines for Documentation
Beyond legal frameworks, medical organisations provide additional documentation standards.
- Consistency: Guidelines from bodies like the World Health Organization (WHO) or national medical associations ensure uniformity across healthcare providers.
- Quality assurance: These standards help maintain compliant and clinically valuable records.
With clear rules, let’s focus on ensuring data safety in electronic health records.
Data Safety and Security in Electronic Records
Protecting patient data isn’t just about following rules—it’s about using the right systems and tools to keep information secure and accessible only to the right people.
1. Strong Regulatory Oversight
Governments and organisations implement strict measures to protect health records.
- Regular audits: Hospitals must undergo regular inspections to ensure compliance with data protection laws.
- Encryption: All data stored in or transmitted through digital health systems must be encrypted to prevent unauthorised access.
2. Avoid Non-Secure Channels
Sharing patient data through unprotected platforms is prohibited, and for good reason.
- Example: Instead of emailing sensitive patient information, healthcare providers communicate using secure portals or encrypted messaging systems.
- Access logging: Every access to a patient’s record is tracked to identify and address any unauthorised activity.
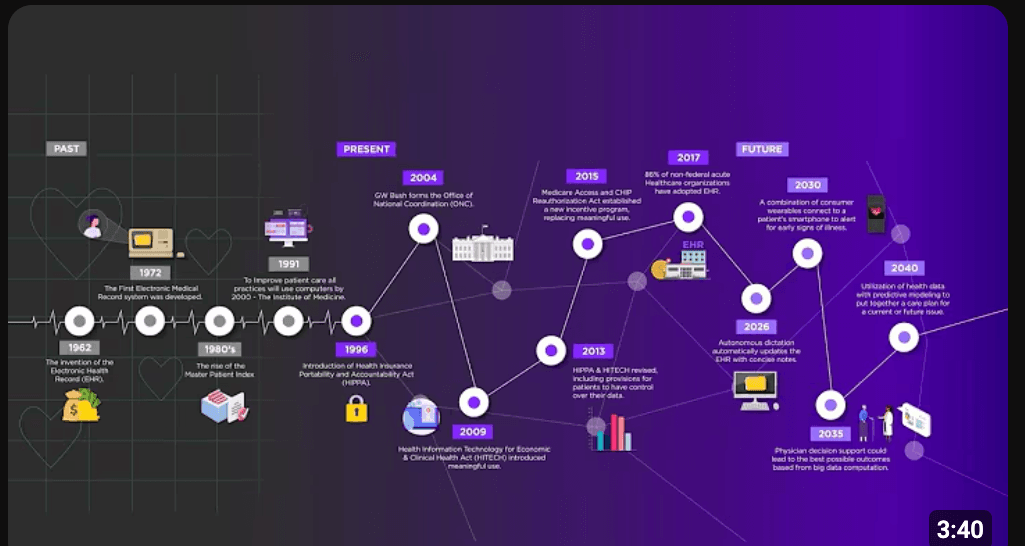
If you want to learn more about digital or electronic health records, including their past, present, and future, here is an interesting video from Extreme Networks.
Conclusion
Digital health records are changing how hospitals and clinics manage patient information. By giving healthcare professionals quick and reliable access to patient data, they improve decision-making, streamline workflows, and enhance the overall quality of care. These systems help reduce errors, ensure better team coordination, and make healthcare delivery smoother and more effective.
At Practaluma, we create digital health record solutions that genuinely work for healthcare professionals. Our systems are built to:
- Simplify workflows: This allows you to spend less time managing data and more time caring for patients.
- Improve decision-making: Provide accurate, real-time information for better care.
- Ensure data protection: Keep sensitive information secure with advanced safeguards.
- Meet compliance needs: Align with global and local regulations with ease.
If your current system feels outdated or inefficient, we’re here to help. Practaluma’s tailored solutions fit your hospital’s needs, allowing you to deliver efficient, organised, and patient-focused care.