5 May 2025
Differences Between Psychotherapy Notes and Clinical Progress Notes
As a healthcare professional, you understand that accurate documentation is crucial for delivering quality care and ensuring compliance with regulations. A study found that more than 80% of diagnostic errors are preventable, often linked to issues in clinical documentation.
Psychotherapy notes, often referred to as process notes, are distinct from clinical notes. While psychotherapy notes are personal reflections used by therapists to track their observations and thoughts during therapy sessions, clinical notes focus on the broader medical context, recording diagnoses, treatment plans, and progress summaries.
But the distinction between psychotherapy and clinical progress notes isn’t just technical. It’s essential for legal protection and effective patient care. Let’s break it down clearly, practically, and directly relevant to your practice.
Difference Between Psychotherapy and Progress Notes
While both psychotherapy notes and progress notes serve important roles in therapy, their purposes, privacy levels, and use cases differ significantly. A clear comparison can help therapists understand how to use each type effectively while meeting professional and legal standards.
Here’s a detailed breakdown:
Psychotherapy Notes vs. Progress Notes: A Side-by-Side Comparison
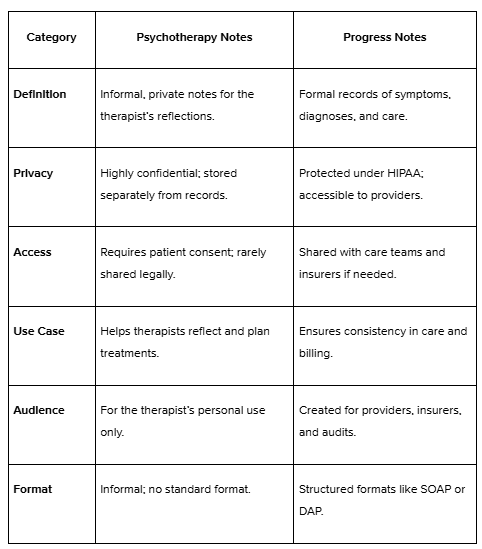
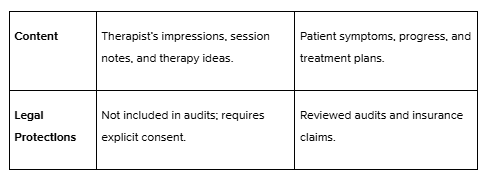
Highlighting the Differences
Psychotherapy notes prioritise privacy and allow therapists to reflect deeply on their patients without concerns about external access. In contrast, progress notes are designed for communication and compliance, ensuring all parties involved in a patient’s care are aligned.
For example, a psychotherapy note might capture, “Consider exploring underlying self-esteem issues related to patient’s perfectionism.” A progress note would instead read, “Patient reports decreased stress after implementing relaxation techniques.”
Now that we’ve explored the key differences between psychotherapy and progress notes, let’s take a closer look at understanding psychotherapy notes.
Understanding Psychotherapy Notes in Detail
Psychotherapy notes are personal reflections used by therapists to document observations, thoughts, and insights during therapy sessions. Unlike clinical records, they are private and meant solely for the therapist’s reference to enhance therapeutic approaches. First things first,
1. What Are Psychotherapy Notes?
Think of psychotherapy notes as your brainstorming journal. They’re where you jot down your thoughts, observations, and hypotheses about a patient’s condition. It’s not about formalities; it’s about capturing the raw, unfiltered insights that come to you during or after a session.
These notes are personal to you. They’re not part of the patient’s medical record but part of your process as a therapist.
2. What Makes Psychotherapy Notes Different?
Psychotherapy notes aren’t just another box to tick. They’re tools that let you dig deeper, plan more brilliantly, and reflect better. Here’s what sets them apart:
- Your Private Thoughts: In these notes, you explore patterns, behaviours, and emotions that might not yet fit into the formal record.
- Questions for Growth: You might write down, “How does this relate to last week’s discussion about trust?” This is a space to plan and probe further.
- Separate from Medical Records: These notes live in their world—apart from the official charts and documentation. That separation allows you to write without worrying about how it looks to anyone else.
3. What is the Privacy Advantage of Psychotherapy Notes?
Here’s where psychotherapy notes shine: Privacy. Under HIPAA, these notes are in a league of their own. They’re protected and can’t be disclosed without the patient’s permission, except for rare situations like a court order.
Why does this matter? Because privacy builds trust. When patients know their most personal thoughts won’t leave the room, they’re more likely to open up—and that’s where the magic of therapy happens.
For instance, if you’re exploring sensitive issues like past trauma, you can document your thoughts freely as you’re building the case formulation, whilst, in the clinical notes, there only needs to be mention of the trauma explored for record purposes. In contrast, clinical notes are part of the patient’s official medical history and must adhere to documentation standards, making them less suited for recording personal reflections or exploratory insights. This distinction offers the kind of security both you and your patient need.
Now that we’ve defined psychotherapy notes, let’s also explore clinical progress notes in detail.
Exploring Clinical Progress Notes
Progress notes play a crucial role in documenting patient clinical care. Unlike psychotherapy notes, which are private and personal to the therapist, progress notes are formal records in the patient’s medical file. These notes ensure clear communication and accountability in patient care.
Defining Progress Notes
Progress notes are official records of the patient’s treatment that capture your observations, clinical findings, and the steps as a therapist to address the patient’s concerns.
What you’ll typically find in progress notes:
- Symptoms: The patient’s reported experiences and issues during the session.
- Clinical Impressions: The therapist assesses the patient’s condition based on the session.
- Treatment Plans: Documented strategies or interventions to address the patient’s needs.
For example, a progress note might state: “Patient-reported improved sleep patterns since the last session. Cognitive behavioural strategies were reviewed and reinforced for managing nighttime anxiety.” This detail ensures the patient’s treatment path is well-documented and traceable.
The Purpose of Progress Notes
Progress notes are designed to do more than keep records—they ensure smooth communication and support the administrative side of therapy.
- Coordinated Care: These notes enable other healthcare providers to understand the treatments provided and the patient’s progress.
- Insurance and Billing: Progress notes verify the services offered and provide evidence for reimbursement purposes. For instance, if a therapist outlines a session’s key takeaways and actions, insurers can confirm that the treatment aligns with the diagnosis and supports payment claims.
Now that we’ve explored what progress notes are and why they’re essential, let’s break down the key components that make them effective and actionable.
Components of Clinical Progress Notes
Progress notes are effective because they follow structured frameworks and include all the vital details necessary for clear communication and documentation. By adhering to these components, therapists ensure that their notes are both professional and functional.
1. Frameworks: Organising Progress Notes
The structure of progress notes helps therapists document sessions logically and consistently. Various frameworks are available, with the most widely used being:
- SOAP (Subjective, Objective, Assessment, Plan): This format organises notes into four sections—what the patient reports (Subjective), observable facts (Objective), the therapist’s analysis (Assessment), and planned actions (Plan).
- DAP (Data, Assessment, Plan): Similar to SOAP but simplified, focusing on session data, professional evaluation, and next steps.
- Other Formats: Depending on the practice, therapists might adopt less rigid frameworks tailored to their specific needs or organisational guidelines.
For instance, a SOAP note might include:
- Subjective: “Patient reports feeling less stressed at work but struggles with sleep.”
- Objective: “Patient appeared calmer today, with improved eye contact.”
- Assessment: “Continued progress with stress management but ongoing issues with insomnia.”
- Plan: “Introduce guided meditation techniques for better sleep.”
2. Contents: What Must Progress Notes Include?
Progress notes aren’t just about structure; their value lies in the content they capture. Every entry should provide a clear picture of the session and its outcomes. Key elements include:
- Session Summaries: A concise overview of what was discussed or addressed during the session.
- Clinical Assessments: The therapist’s interpretation of the patient’s condition or progress.
- Treatment Plans: Details of the interventions used, adjusted strategies, or future steps.
- Patient Progress: An evaluation of how the patient is responding to the treatment over time.
For example, a progress note might summarise a session with:“Reviewed coping strategies for managing workplace anxiety. The patient reported improvement in applying techniques but expressed difficulty during high-pressure moments. Plan to reinforce skills with role-playing scenarios next session.”
With the components of progress notes outlined, it’s time to explore purpose and security of psychotherapy notes..
Purpose of Psychotherapy Notes
Psychotherapy notes serve a dual purpose: they enable therapists to record and process sensitive insights while maintaining the integrity of a patient’s official medical records. Their confidentiality fosters trust, creating a secure space for both reflection and effective therapeutic planning.
Purpose: Why Are Psychotherapy Notes Essential?
Psychotherapy notes allow therapists to reflect on and refine their treatment approach. They are not meant to be shared; they are written solely for the therapist’s benefit.
Here’s what they’re designed to do:
- Develop Treatment Plans: These notes allow therapists to map out strategies based on private reflections, free from the constraints of formal documentation.
- Protect Sensitive Information: Therapists keep delicate observations out of medical records, ensuring that only the most relevant data is shared and maintaining the patient’s privacy.
For instance, a note might say, “Explore deeper connections between their anxiety and past relationships in the next session.” This planning stays private, helping the therapist focus on progress without exposing personal details.
Now that we know the purpose of psychotherapy notes, let’s look at the legal and privacy considerations for the same.
Legal and Privacy Considerations in Documentation
When it comes to documentation, the legal and privacy rules surrounding psychotherapy and progress notes are not the same. These differences impact how they are accessed, shared, and protected, making it crucial for therapists to handle each type with care and precision.
Let’s take a closer look at how legal and privacy considerations apply to both progress notes and psychotherapy notes.
1. Progress Notes: Less Restrictive but Still Regulated
Progress notes are part of the patient’s official medical record and are subject to specific regulations under HIPAA (Health Insurance Portability and Accountability Act). While privacy laws protect them, they are more accessible than psychotherapy notes.
Key points about progress notes:
- Access by Third Parties: Progress notes can be reviewed by insurance companies for billing and reimbursement purposes.
- Legal Audits: They may also be included in audits, court orders, or subpoenas if required.
- Transparency in Care: Because they provide a record of diagnosis and treatment, progress notes are designed to be shared within a patient’s care team to ensure continuity of care.
For example, an insurance company might request progress notes to confirm that a therapy session aligns with the billed service and diagnosis.
2. Psychotherapy Notes: Highly Confidential
Psychotherapy notes are treated with much stricter privacy protections. These notes are excluded from the patient’s medical record and require explicit consent from the patient to be shared.
Key points about psychotherapy notes:
- Explicit Authorisation: Unlike progress notes, psychotherapy notes cannot be disclosed without the patient’s written authorisation, except in rare cases, such as a legal mandate.
- Exemption from Audits: Psychotherapy notes are not subject to routine audits by insurance companies or included in legal proceedings unless a court order specifically demands them.
- Encouraging Openness: This heightened level of confidentiality encourages patients to share deeply personal thoughts, knowing they remain private.
For instance, a therapist’s private reflections about a patient’s underlying fears or unresolved trauma would remain confidential, even during a legal dispute, unless a specific legal exception applies.
To know more about the difference between psychotherapy and clinical progress notes, here is a YouTube video by Psychology in Seatle that helps you understand better visually.

Conclusion
The differences between psychotherapy notes and progress notes highlight their distinct roles in therapy. Psychotherapy notes provide a private space for therapists to reflect and strategise, fostering deeper insights and more effective treatment plans. On the other hand, progress notes ensure continuity of care, support administrative processes, and maintain transparency across healthcare teams.
Mastering both types of documentation allows therapists to strike the perfect balance—ensuring patient trust, meeting legal standards, and delivering exceptional care.
Ready to Elevate Your Documentation Skills?
At Practaluma, we’re here to help therapists like you refine your practice with tools, training, and resources that simplify and strengthen your work. Here’s how we can help:
1. Comprehensive Training Programs: Learn the art of precise, professional documentation with expert-led workshops tailored to psychotherapy and progress notes.
2. Personalised Mentorship: Get one-on-one guidance from experienced professionals to navigate complex cases and ensure your documentation meets both clinical and legal standards.
3. Cutting-Edge Resources: Access templates, examples, and best practices for creating notes that are efficient, accurate, and compliant.
4. Community Support: Join a network of therapists who share insights, challenges, and solutions to grow together.
Visit Practaluma to explore our programs and tools. Whether you’re new to therapy or looking to sharpen your skills, we’re here to help you master the art of documentation. Sign up for a free consultation or register for our upcoming workshops today.