19 March 2025
SOAP Note Templates for Mental Health Counseling: Examples and Tips
Accurate and structured documentation is a fundamental aspect of mental health counselling. SOAP notes—a standardised format encompassing Subjective, Objective, Assessment, and Plan—provide clinicians with an efficient method for recording patient progress, formulating treatment plans, and ensuring regulatory compliance.
This blog explores how SOAP note templates can enhance your mental health practice. From detailed examples for conditions like anxiety and depression to practical tips on improving note-taking accuracy, this guide is designed to support mental health professionals in delivering consistent, high-quality care.
Understanding SOAP Notes
SOAP notes stand for Subjective, Objective, Assessment, and Plan. They are a structured framework for clearly and systematically documenting patient interactions. Originating in medical practices, this format has become a cornerstone in mental health counselling, enabling professionals to record client information systematically.
Purpose of SOAP NotesThe primary purpose of SOAP notes is to ensure that each session’s details are documented logically and consistently. By structuring notes into clear categories, clinicians can track patient progress over time, providing a reliable reference for treatment decisions and professional communication.
Understanding the purpose of SOAP notes is essential, but why is this structure so crucial to clinical practice? Let’s explore its broader significance in mental health counselling.
Importance of SOAP Notes
SOAP notes play a vital role in mental health counselling by providing a structured and reliable framework for documentation. Their importance extends beyond record-keeping, impacting communication, compliance, and the overall quality of care.
1. Structured Framework
SOAP notes provide a uniform structure that simplifies the documentation process. By organising information into distinct categories—Subjective, Objective, Assessment, and Plan—clinicians can ensure that each detail is recorded systematically. This structured approach reduces errors, enhances efficiency, and supports consistent care delivery.
2. Improved Communication
Clear and organised SOAP notes are invaluable for communication among healthcare providers. They serve as a professional record that ensures all team members can access accurate, up-to-date information about a patient’s progress and treatment plan. This improves collaboration and reduces the risk of miscommunication, particularly in multidisciplinary teams.
3. Legal and Ethical Compliance
Maintaining comprehensive SOAP notes is critical for meeting regulatory and ethical standards in mental health counselling. Detailed documentation safeguards the clinician and the patient, providing a clear care account. SOAP notes can be crucial evidence of appropriate treatment and decision-making in audits, legal inquiries, or insurance reviews.
Now that we’ve highlighted the significance of SOAP notes let’s explore practical tips for writing adequate and professional documentation.
Tips for Writing Effective SOAP Notes
Clear and professional SOAP notes are essential for accurate and actionable clinical documentation. These tips, accompanied by real-life examples, will help you streamline your note-taking process while upholding the highest standards in mental health counselling.
1. Timely Documentation
Document SOAP notes immediately after each session to ensure they are accurate and comprehensive. Waiting too long can lead to missing essential details or including inaccuracies that may affect care decisions.Example: After a session with a client experiencing post-traumatic stress, you document their self-reported nightmares and flashbacks (Subjective) and note observable signs of hypervigilance, such as scanning the room frequently (Objective).
2. Professional Language
Use concise and professional language, avoiding casual expressions or overly technical jargon. This ensures clarity and makes your notes accessible to other professionals involved in the client’s care.Example: Instead of writing “The client was really on edge,” document “The client displayed heightened alertness and frequent scanning of the environment, consistent with hypervigilance.”
3. Objective Reporting
Focus on factual observations and avoid assumptions or emotional interpretations. Reliable and unbiased notes support sound clinical decisions and enhance collaboration among care providers.
Example: Record observations like “The client had a rigid posture and spoke in a low, monotone voice” rather than “The client appeared depressed.”
Armed with these tips, let’s explore the structure of SOAP notes and how each section contributes to creating thorough and adequate documentation.
With the structure of SOAP notes outlined, it’s equally important to understand and avoid common mistakes that compromise documentation quality. Let’s discuss these next.
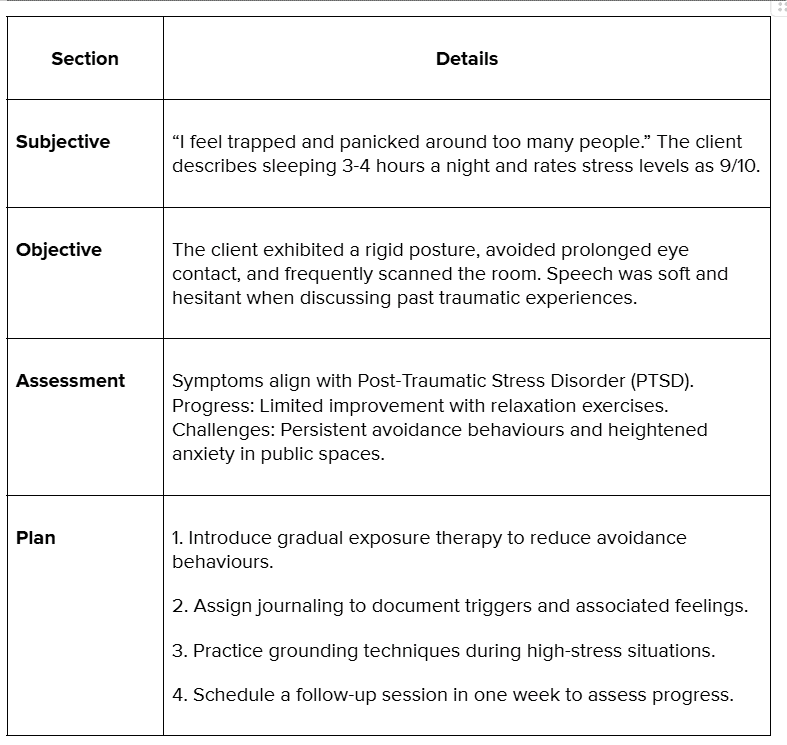
SOAP Note Templates and Examples

SOAP note templates are invaluable tools for ensuring consistency and thoroughness in documentation. Below are tailored templates and examples for common mental health scenarios, highlighting how to apply the SOAP format in practice effectively
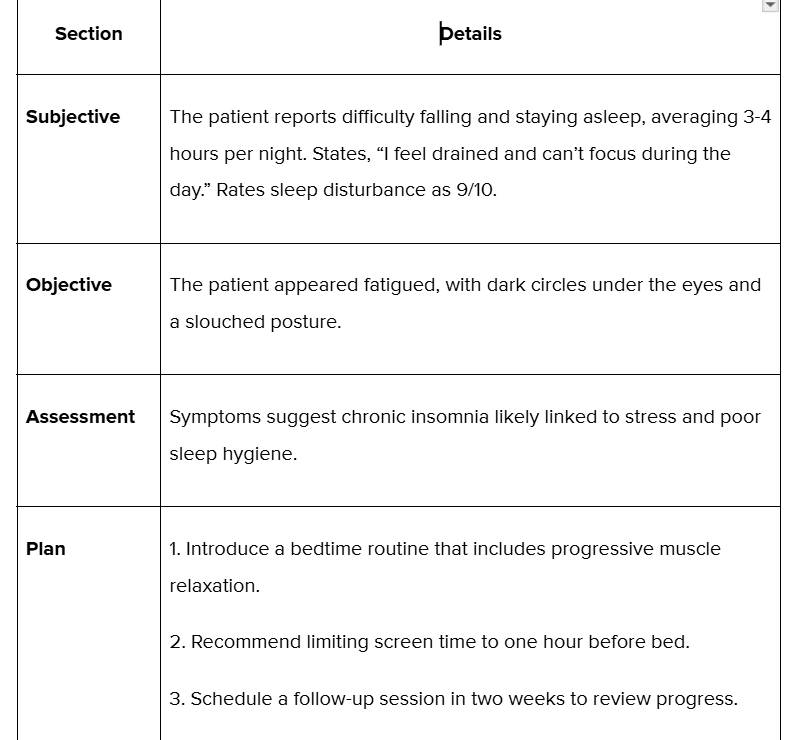
Example 1: Insomnia (Chronic Sleep Disturbance)
Let’s consider another example with respect to Depression and mental health documentation.
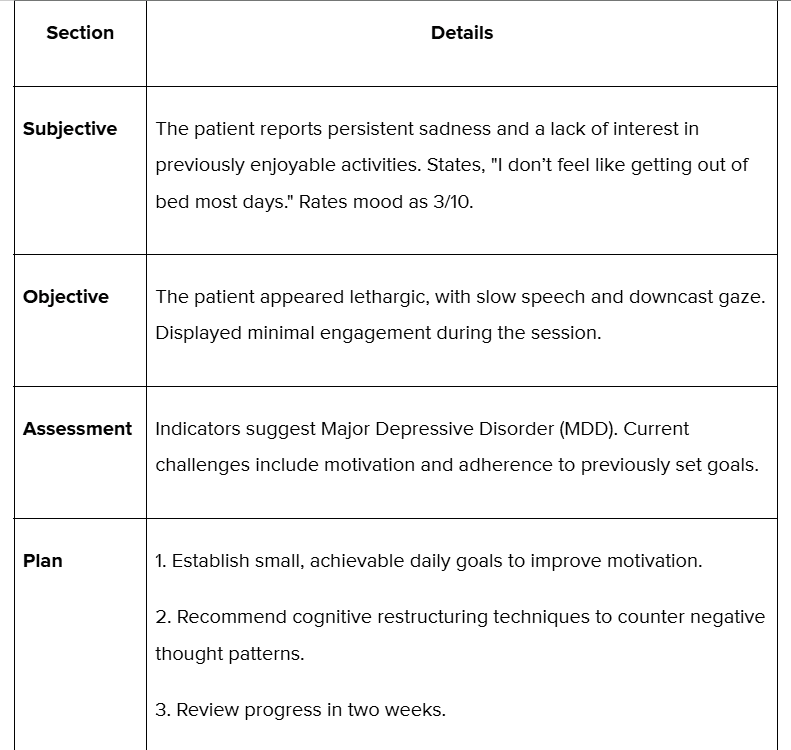
Example 2: Depression (Major Depressive Disorder)
Let’s also consider a SOAP note example for a short-term counselling session.
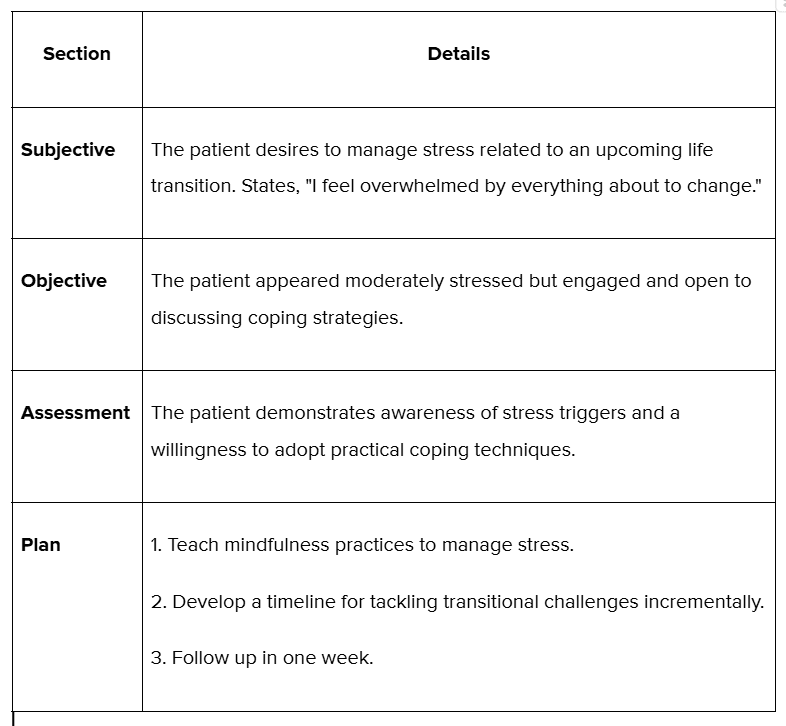
Example 3: Short-Term Counseling Goals
Now that we’ve established tips for practical SOAP notes, let’s examine their structure in greater detail to understand how each section contributes to accurate and actionable documentation.
The Structure of a SOAP Note
A well-written SOAP note is divided into four sections: Subjective, Objective, Assessment, and Plan. Each component serves a specific purpose in capturing patient details comprehensively and logically. Here’s a detailed breakdown of each section:
Subjective (S)The subjective section captures the patient’s personal experiences, concerns, and reported symptoms. It provides insight into the patient's perspective on their condition and helps us understand their overall state.Example:The patient states, “I feel overwhelmed and have difficulty focusing on tasks at work.”Reports frequent headaches and fatigue, with sleep averaging 4-5 hours per night.
Objective (O)This section documents observable and measurable data collected during the session. It includes physical findings, clinician observations, and any relevant diagnostic information.Example:The patient appeared distracted, with difficulty maintaining focus during the session.Displayed a slouched posture and rubbed their temples frequently, reporting mild headache pain (self-rated 5/10).
Assessment (A)The assessment involves synthesising subjective and objective data to form a clinical impression. It highlights the clinician’s interpretation and any relevant diagnostic insights.Example:Symptoms suggest work-related stress contributing to mild anxiety and physical tension—minimal progress was observed in managing workload pressures, indicating a need for additional stress-reduction techniques.
Plan (P)The plan outlines actionable steps for treatment and follow-up care. It ensures continuity and addresses patient goals for the future.Example:
- Introduce time management strategies to address workload stress.
- Recommend a daily stretching routine to alleviate physical tension.
- Encourage keeping a stress journal to identify recurring patterns.
- Schedule a follow-up session in one week to review progress and refine coping strategies.
Let us explore some common mistakes that can happen while writing SOAP notes.
Common Mistakes in SOAP Notes
Despite the structured nature of SOAP notes, inevitable mistakes can undermine their effectiveness. Awareness of these common errors can help clinicians maintain the quality and accuracy of their documentation.
1. Lack of Specificity
Using vague language reduces the clarity and usefulness of SOAP notes. Precise details ensure that other healthcare professionals can understand the patient’s condition and progress without ambiguity.An example of a mistake is writing “The patient seems anxious” instead of “The patient appeared restless, exhibited rapid speech, and frequently fidgeted during the session.”Correction: Include measurable observations or specific examples to avoid misinterpretation.
2. Ignoring Direct Quotes
Patient statements provide valuable insight into their experiences and emotions. Omitting direct quotes can result in losing context or key details about their condition.Example of a mistake: Summarising “Patient feels stressed” instead of quoting, “I feel like I’m carrying the weight of the world on my shoulders.”Correction: Integrate direct quotes where applicable to accurately capture the patient’s perspective.
3. Omitting Key Details
Adding essential elements, such as specific symptoms or treatment steps, can lead to complete documentation, compromising the SOAP note's usefulness for current treatment and future reference.An example of a mistake is failing to document follow-up plans after an assessment.Correction: Always ensure each section—Subjective, Objective, Assessment, and Plan—is thoroughly addressed with no gaps.
4. Overuse of Jargon
While SOAP notes are meant for professional communication, excessive medical jargon can make them harder to interpret. Documentation should balance professionalism with accessibility.An example of a mistake is writing “The patient displayed paroxysmal nocturnal dyspnoea” instead of “The patient reported shortness of breath at night.”Correction: Use clear, professional language that is understandable across disciplines.
Addressing these common errors is important for maintaining accurate and effective documentation, ensuring optimal patient care and facilitating seamless communication within your healthcare team.
Conclusion
SOAP notes are essential in mental health counselling, offering a structured, consistent approach to documenting patient interactions. By breaking down information into clear categories—Subjective, Objective, Assessment, and Plan—clinicians can provide better continuity of care, improve communication among professionals, and ensure compliance with legal and ethical standards. Accurate and thorough documentation benefits the patient and enhances the efficiency and effectiveness of the healthcare system.
Adequate documentation is the foundation of successful mental health counselling, and Practaluma is here to support you every step of the way. Our tailored solutions are designed to make your SOAP notes more precise, efficient, and compliant with healthcare standards.
Why Choose Practaluma ?
- Custom SOAP Note Templates: Access professionally designed templates for anxiety, depression, and more, ensuring every detail is covered.
- Training and Support: Learn best practices for crafting accurate SOAP notes through our expert-led workshops and resources.
- Digital Integration Solutions: With our guidance, you can seamlessly incorporate SOAP notes into your existing EHR systems or explore new digital platforms.
- Regulatory Compliance: Stay ahead of legal and ethical requirements with documentation solutions aligned to Australian healthcare standards.
- 24/7 Assistance: Our team of experts is here to answer your questions and provide ongoing support whenever needed.
Ready to transform your documentation process?Contact us today to schedule a consultation or explore our range of services. Let us help you focus on what truly matters—your patients’ well-being.