19 March 2025
How to Write GIRP Notes with Example and Template
GIRP notes are structured to document therapeutic interactions, focusing on goals, interventions, responses, and plans.
Clinical documentation is not just an administrative task—it serves as the foundation of effective therapy. Among the various note formats, GIRP notes stand out for their comprehensive framework, enabling practitioners to track progress systematically and tailor future interventions effectively.
In this blog, we’ll explore the essentials of GIRP notes, including their structure, practical applications, and benefits. Whether you’re new to this format or looking to refine your documentation skills, this guide will equip you with the tools to write clear, practical, and actionable GIRP notes.
Understanding GIRP Notes
GIRP notes are a type of clinical documentation that follows a structured framework: Goals, Intervention, Response, and Plan. This format is designed to help therapists document their sessions systematically, ensuring that each note captures the essential elements of therapeutic interactions.
1. Structure and Benefits
The structure of GIRP notes makes them especially effective for tracking progress. By breaking down each session into precise components, these notes:
- Clarify Therapy Objectives: Provide clarity on the goals and purpose of therapy.
- Document Interventions and Outcomes: Offer a detailed record of interventions and their results.
- Enhance Collaboration: Facilitate effective communication and collaboration among care providers.
- Support Treatment Adjustments: Serve as a valuable reference for modifying treatment plans based on client progress.
2. Comparison with Other Formats
Unlike SOAP or BIRP notes, GIRP notes emphasise goal-setting and measurable outcomes more strongly. While SOAP focuses on subjective and objective observations, and BIRP is intervention-driven, GIRP integrates these elements with an outcome-oriented perspective, making it particularly suited for therapy-focused documentation.
With a solid understanding of GIRP notes, let’s explore the components that make this framework practical and versatile for therapeutic documentation.
Components of GIRP Notes
As we are pretty aware, GIRP notes are organised into four key sections: Goals, Intervention, Response, and Plan. Each component plays a vital role in capturing the essence of a therapy session and guiding the therapeutic process.
1. Goals
The “Goals” section outlines the objectives of the therapy session or Overall treatment plan. These goals provide direction for interventions and set measurable benchmarks for progress.
- Purpose: To establish a precise therapeutic aim, aligning the session with the client’s objectives.
- Example: “Reduce the intensity of anxiety symptoms from 8/10 to 5/10 over the next month through relaxation techniques.”
2. Intervention
The “Intervention” section details the therapist’s actions during the session, including techniques, strategies, or exercises to address the goals.
- Purpose: To document and link the therapeutic approaches directly to the client’s goals.
- Example: “Guided the client through a 10-minute progressive muscle relaxation exercise to manage anxiety symptoms.”
3. Response
The “Response” section captures the client’s reaction to the interventions. This can include emotional, behavioural, or verbal responses and observable changes during the session.
- Purpose: To assess the client’s progress and gather insights for refining interventions.
- Example: “Client reported feeling calmer after the relaxation exercise and expressed willingness to practice it at home.”
4. Plan
The “Plan” section outlines the next steps in therapy, including follow-up activities, assigned homework, or adjustments to the treatment plan.
- Purpose: To ensure continuity of care and provide a roadmap for future sessions.
- Example: “Assign daily relaxation practice for 10 minutes and review progress during the next session.”
Now that we’ve broken down the components of GIRP notes, let’s examine how to define and document clear, practical goals in therapy.
Writing Clear and Effective Goals in GIRP
Setting clear goals is the foundation of effective therapy and well-documented GIRP notes. Well-defined goals guide interventions, measure progress, and provide a roadmap for the therapist and the client.
1. Importance of Defining Goals in Therapy
Goals help focus the therapeutic process, ensuring each session has a clear purpose. They offer the therapist and the client measurable benchmarks to assess progress and adjust the treatment plan as needed.
Example: Instead of vague goals like “reduce stress,” specify “reduce the frequency of stress-related headaches from daily to twice a week within one month.”
2. Using SMART Criteria for Goal Setting
The SMART framework is an effective tool for creating actionable and measurable therapy goals:
- Specific: Clearly define what the goal aims to achieve.
- Measurable: Include metrics to track progress.
- Achievable: Set realistic goals based on the client’s abilities.
- Relevant: Align the goal with the client’s broader objectives.
- Time-bound: Set a timeline for achieving the goal.
Example: “Increase social interactions by initiating a conversation with at least one new person per week for the next month.”
3. Short-Term vs. Long-Term Goals
In therapy, it’s crucial to balance short-term and long-term goals:
- Short-Term Goals: Focus on immediate, actionable steps that build momentum.
Example: “Practice deep-breathing exercises daily to reduce anxiety during stressful situations.”
- Long-Term Goals: Aim for overarching outcomes that reflect significant progress.
Example: “Develop consistent coping mechanisms to manage anxiety in public settings within six months.”
With clear and actionable goals in place, the next step is documenting the interventions used during therapy sessions to achieve these objectives.
Documenting Interventions
The intervention section of GIRP notes records the therapeutic techniques and actions taken during a session. This component connects directly to the client’s goals and helps create a clear picture of therapy progress.
1. Purpose of the Intervention Section
The intervention section ensures that every therapeutic action is documented systematically. It highlights the strategies used by the therapist and their relevance to the client’s goals, providing a detailed account of the care provided.
2. Best Practices for Recording Interventions
Follow these principles to document interventions clearly and professionally:
- Specificity: Record precise details about the techniques or strategies used.
- Objectivity: Describe what was done factually, without subjective interpretation.
- Goal Alignment: Ensure interventions directly address the goals outlined in the client’s treatment plan.
- Action-Oriented Language: To describe the therapist's role, use strong, active verbs like “taught,” “guided,” or “demonstrated.”
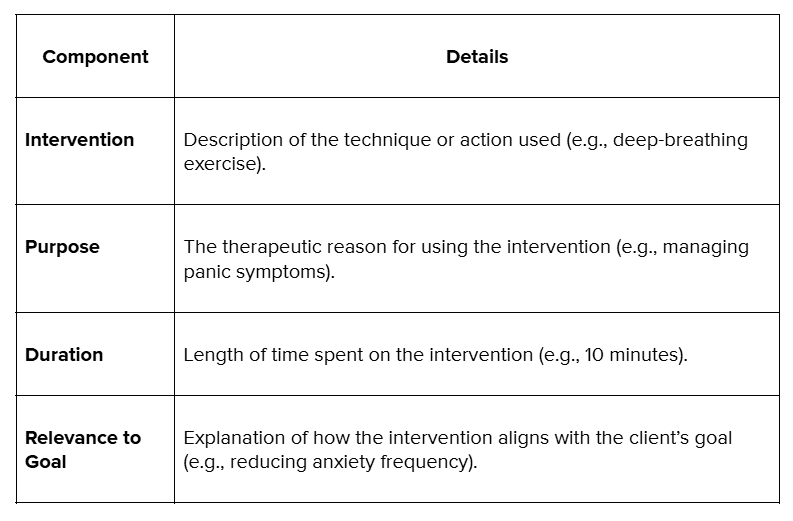
3. Sample Table for Documenting Interventions
Here’s a structured approach to recording interventions in GIRP notes:
Once the interventions are documented, the next step is to record the clients' responses to assess the session's impact.
Capturing Client Responses
Client responses are the heart of GIRP notes. This section captures how clients react to the interventions, offering a clear window into their progress and challenges. Accurate and objective documentation of these responses helps therapists refine their strategies and adjust treatment plans effectively.
1. Focus on Reactions, Not Assumptions
The client’s response section should document what was observed or reported during the session. Avoid making assumptions or interpretations; stick to the facts. This clarity ensures that every note remains professional and actionable.
2. Precision Over Generalization
Details matter. Generic phrases like “client responded well” don’t tell the whole story. Instead, focus on specifics: how did the client engage with the intervention? Were there measurable changes? Did they express any thoughts or feelings that are significant to their progress?
3. Use Direct Quotes for Impact
Nothing captures the essence of a session like a client’s own words. Direct quotes provide context, add authenticity, and serve as a powerful reference for evaluating progress. For instance, noting a client’s statement, such as, “I feel like I can finally breathe easier,” is far more impactful than a general observation.
4. Objective Documentation for Accuracy
Every response recorded should be factual and unbiased. This approach ensures consistency and creates a reliable record that can be shared among care providers or referenced in reviews.
Developing a Comprehensive Plan
The plan section of GIRP notes outlines the next steps in the client’s therapeutic journey. It ensures continuity of care by detailing follow-up actions, homework assignments, and adjustments to the treatment plan based on the client’s progress.
1. Outlining Next Steps for Therapy
A strong plan provides a clear direction for both the therapist and the client. It specifies what will be addressed in upcoming sessions, ensuring that therapy remains goal-oriented and focused.
- For example, setting a goal to introduce new relaxation techniques or refine previously learned skills in the next session.
2. Assigning Homework or Follow-Up Activities
Assigning tasks for clients to complete between sessions encourages active participation and reinforces the progress made during therapy. These activities should align with the session’s goals and be achievable within the client’s context.
Examples of homework are practising coping strategies, journaling thoughts, or engaging in mindfulness exercises.
3. Adjusting Plans Based on Client Progress
The plan should reflect the client’s evolving needs and progress. Regularly reviewing and updating the plan ensures that therapy remains effective and adaptive.
- If a goal has been achieved, set new challenges. If progress is slower than expected, explore alternative interventions or approaches.
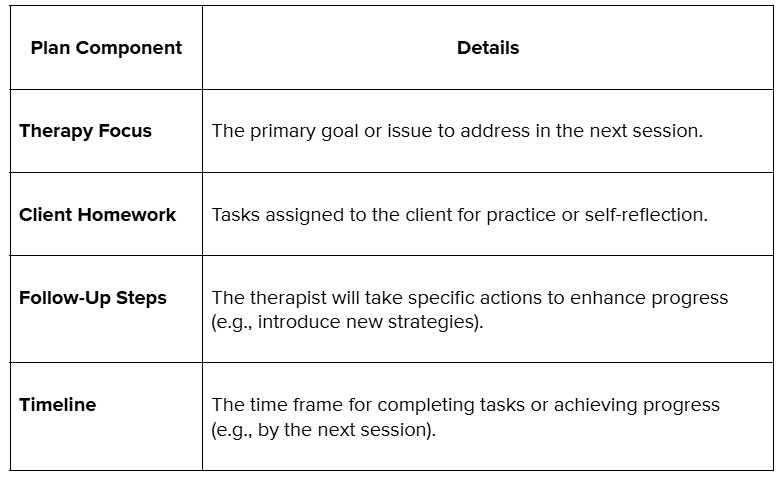
Elements of an Effective Plan
With the comprehensive plan components outlined, let’s combine everything with a complete example of a structured GIRP note.
A Solid Example of a GIRP Note
Below is a detailed example of a structured GIRP note for a therapy session focused on managing anxiety. This example demonstrates how to document each section effectively.
Date and Time: 18 December 2024, 3:00 PMTherapist Name: Dr. Sarah Johnson, Licensed Clinical PsychologistSession Number: 5
G: Goals
The session aimed to help the client reduce the intensity of anxiety symptoms during stressful situations.
- Short-Term Goal: Practice relaxation techniques to manage physical symptoms of anxiety, such as rapid heart rate and shallow breathing.
- Long-Term Goal: Develop confidence in handling social interactions independently within three months.
I: Intervention
The therapist introduced and guided the client through progressive muscle relaxation (PMR) exercises during the session. This technique was selected to address the client’s immediate physical anxiety symptoms and enhance emotional regulation.
- Duration: 15 minutes
- Approach: Step-by-step instructions for PMR focus on recognising and releasing muscle tension in the body.
- Context: Discussed scenarios where the client could apply PMR techniques independently, such as before a presentation or during a social event.
R: Response
The client appeared engaged and followed the PMR instructions with minimal difficulty.
- Reported feeling “lighter” and “more in control” after completing the exercise.
- Observed Response: The client’s posture visibly relaxed, and their breathing slowed significantly by the end of the session.
- Client Feedback: Expressed interest in continuing to use PMR techniques, stating, “I think this could help me in high-pressure situations.”
P: Plan
The therapist and client collaborated to outline the following steps:
- Assign homework: Practice PMR for 10 minutes daily and document experiences in a journal.
- Plan for the next session: Review journal entries, address challenges in practising PMR, and introduce cognitive reframing techniques.
- Timeline: Evaluate progress during the next session, scheduled for 25 December 2024.
Conclusion
GIRP notes are more than a documentation tool—they’re a critical part of the therapeutic process. By organising notes into Goals, Interventions, Responses, and Plans, therapists can create a structured record that supports client progress, facilitates communication among care providers, and ensures compliance with professional standards.
Managing clinical notes like GIRP can be time-consuming, but it doesn’t have to be. At Practaluma, we offer tailored solutions to help therapists and care providers streamline their documentation processes, saving time while maintaining professional standards.
How Practaluma Can Improve the Effectiveness and Efficiency of Writing GIRP Notes
- Custom Templates for GIRP Notes: Access professionally designed templates that align with therapeutic best practices, ensuring transparent and compliant records.
- Training and Workshops: Learn how to write precise and effective notes with guidance from industry experts.
- Digital Documentation Solutions: Leverage user-friendly electronic systems to organise, store, and retrieve clinical notes securely.
- Compliance Support: We will ensure that your notes meet all legal and ethical requirements, reducing the risk of audits or disputes.
- 24/7 Support: Our dedicated team can assist you with any documentation-related questions or challenges.
Ready to get started?Contact us today to learn more about our services and how we can support your practice. Let us help you document with confidence and care.