1 April 2025
Writing Aged Care Nursing Progress Notes - With Examples
As a doctor or a psychologist in old age care, your role involves more than just providing physical care. It also requires accurate, timely documentation to ensure patient safety and continuity of care. Nursing progress notes are crucial in this process, serving as a detailed record of a patient’s condition, treatment, and responses to care.
These notes are essential for delivering consistent care and help protect patients and doctors, ensuring legal compliance and clear communication across care teams.
What are Aged Care Nursing Progress Notes?
Nursing progress notes are written records documenting a patient's condition, treatment, and the care provided during their time in a healthcare facility.
In aged care, where patients often experience multiple chronic conditions, these notes are especially vital for tracking health changes and managing complex treatment plans.
Primary Purpose:
- Track health status and document treatment interventions.
- Ensure continuity of care across shifts and healthcare providers.
- Provide a clear, accurate record of care delivered.
These progress notes are the backbone of patient care in aged care settings, helping ensure that each healthcare provider has the most current and accurate information.
The Role and Importance of Nursing Progress Notes
Nursing progress notes are essential for documenting care across all healthcare settings, but they are particularly significant in aged care due to the complex medical needs of elderly patients. These notes help healthcare professionals track the following:
- Trends in health (e.g., changes in vital signs, mental status).
- Responses to treatments (e.g., improvements or adverse reactions).
- Necessary adjustments to care plans based on evolving patient needs.
Proper documentation of these changes allows for better clinical decision-making, improves patient outcomes, and ensures continuity of care. Additionally, progress notes serve as a legal and communication tool, providing evidence of care and documenting any incidents or changes in a patient’s condition.
Now that we know what nursing progress notes are, let us explore some of the best practices for writing them.
Best Practices in Writing Nursing Progress Notes
Let's now look closer at how to write nursing progress notes effectively, building on their fundamental purpose and importance. Following best practices ensures that your documentation is comprehensive and accurate, improving patient care.
1. Timely and Real-Time Updates at the End of Shifts
Document observations at the end of your shift or as events occur. Timely documentation captures the most current patient information, which is critical for ongoing care.
2. Detail-Oriented and Factual Documentation
Your nursing progress notes should be objective and based on facts. Focus on observable data and measurable outcomes, such as:
- Vital signs check (e.g., blood pressure, pulse, temperature).
- Specific treatments and medications were administered.
- The patient’s responses to care and any significant changes in their condition.
Avoid subjective statements like “Patient seems better.” Instead, document specific facts: "Patient’s skin tone improved after receiving 500 ml of IV fluids."
3. Using Active Voice, Specificity, and Objectivity
Use the active voice to convey clearly who performed each action. For Example: "Administered 5 mg of lorazepam orally at 10:00 AM as per the prescribed dosage, with the patient reporting a decrease in anxiety within 20 minutes."
1. Specificity: Avoid vague language. Be precise with your descriptions, including times, doses, and actions taken.
2. Objectivity: Stick to your observations and avoid personal opinions or assumptions. Document exactly what happened, focusing on measurable outcomes.
Understanding the diverse components of nursing progress notes is essential, and we will delve into this critical topic in the next section.
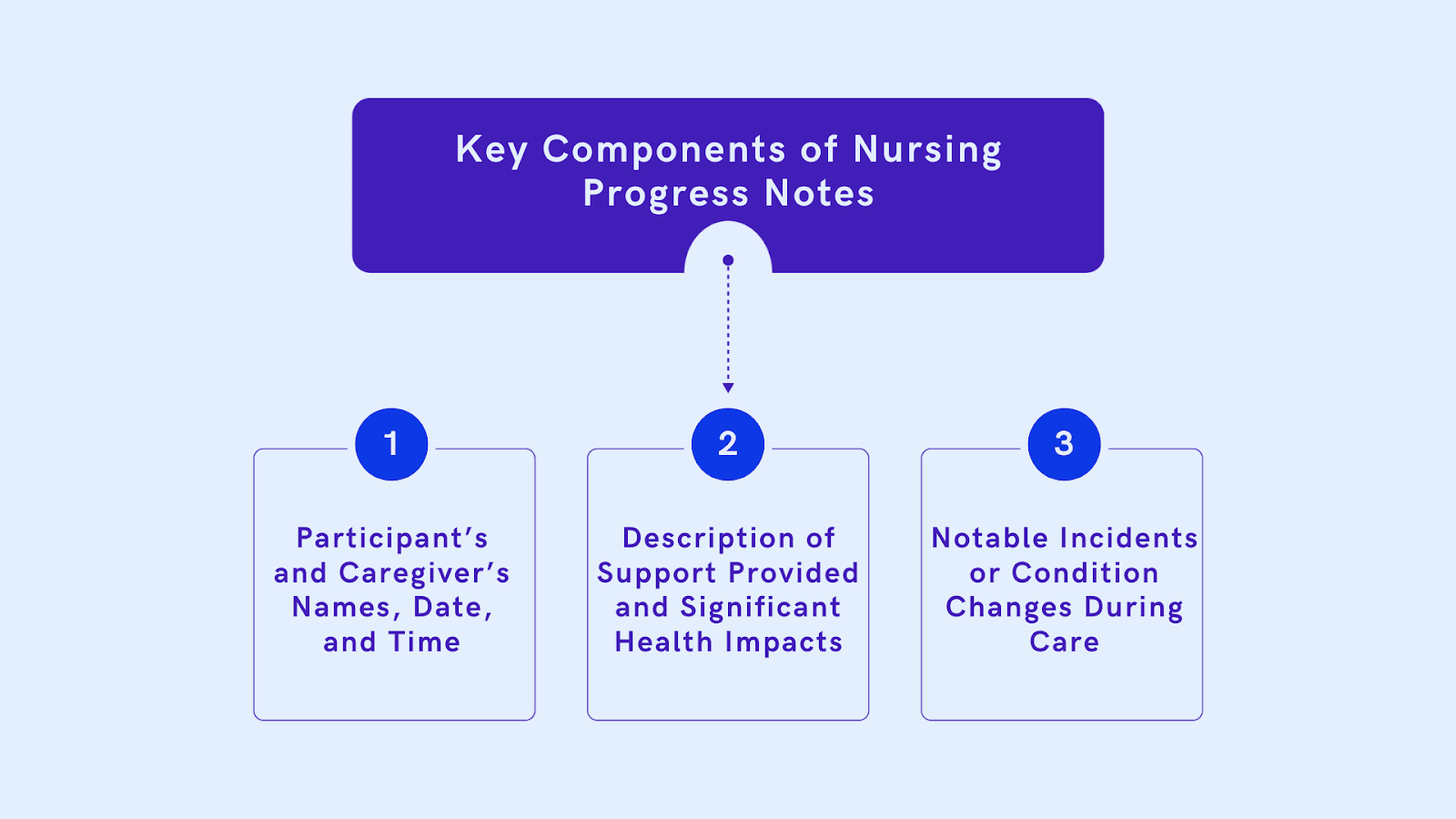
Key Components of Nursing Progress Notes
Nursing progress notes are key to tracking a patient’s journey and ensuring quality care. The main components include documenting the patient’s condition, treatments administered, and how they respond to those treatments. It’s also important to note any changes in their status and adjust the care plan accordingly. These key details help keep the whole care team aligned and focused on the patient's needs.
1. Participant’s and Caregiver’s Names, Date, and Time
Each progress note should include the following:
- Patient’s Name
- Caregiver’s Name
- Date and Time of Documentation
This ensures the note is properly attributed and time-stamped for future reference.
2. Description of Support Provided and Significant Health Impacts
Document what services were provided, including:
- Medications were administered, treatments were given, and any mobility assistance was provided.
- Significant changes in the patient’s condition, such as improvements or deterioration.
3. Notable Incidents or Condition Changes During Care
If there were any changes in the patient’s condition or notable incidents, these should be recorded in detail:
- Was there a positive or negative change in health?
- Were there any unexpected developments, such as a fall or adverse reaction to medication?
Models and Methodologies for Writing Nursing Progress Notes

To help structure your notes efficiently, consider using models like SOAP or STAR. These models provide a clear, systematic way to document patient information.
SOAP (Subjective, Objective, Assessment, Plan)
This model breaks down your notes into clear sections, allowing for organised documentation.
SOAP Example:
- Subjective: The patient reports pain in the lower back.
- Objective: Pain level at 6/10 on the scale.
- Assessment: Likely musculoskeletal pain.
- Plan: Administer pain reliever as prescribed and monitor for improvement.
STAR (Situation, Task, Action, Result)
This model helps structure your approach to problem-solving or performance reviews by clearly outlining the context, the objectives, the steps taken, and the outcomes.
STAR Example:
- Situation: The team faced a tight deadline to deliver a client presentation.
- Task: I created a visually appealing, informative slide deck.
- Action: I collaborated with the design team to ensure the slides were aesthetically pleasing and aligned with the client’s expectations while streamlining the content to fit the time frame.
- Result: The presentation was delivered on time, and the client praised the clarity and design, leading to a follow-up project.
To better understand how to apply these key components, let's walk through a nursing progress note example.
Practical Example of Nursing Progress Notes.
Now that we’ve covered the critical components of a good nursing progress note let’s move on to how these elements can be implemented using structured templates and examples.
Example of a Nursing Progress Note
- Date: April 21, 2024
- Time: 10:30 AM
- Patient Age: 65 Years.
- Patient Name: John Doe
- Caregiver/Author: Nurse Jane Smith
- Shift: Morning
Subjective:
- Patient’s Reported Symptoms: The patient reported feeling very dizzy and light-headed after breakfast.
- Family Input: The daughter mentioned that the patient has been more tired than usual for the past two days.
Objective:
- Physical Observations: Blood pressure 140/85 mmHg, pulse 95 bpm, respirations 18 breaths/min. No signs of swelling or bruising.
- Clinical Data: Recent lab results: Sodium level average, potassium level low.
- Interventions/Actions Taken: Administered prescribed anti-dizziness medication (Meclizine 25 mg). Encouraged hydration and notified the attending physician about the change in symptoms.
Assessment:
- Nursing Assessment: The patient is experiencing symptoms consistent with low potassium. Dizziness may be linked to electrolyte imbalance, supported by lab results.
- Diagnosis/Problems Identified: Risk of electrolyte imbalance and dehydration.
Plan:
- Next Steps: Continue to monitor vital signs every 4 hours. Administer potassium supplements as prescribed.
- Follow-Up Care: Recheck lab results in 24 hours. Review with the attending physician for possible medication adjustments.
- Communication with Other Providers: Notified the attending physician of the patient’s symptoms and low potassium levels. She was awaiting further orders.
With this example in mind, properly handling sensitive patient information is critical. Data privacy remains a top concern, especially when medical details are at risk of being misused. Let's explore some secure documentation practices to protect patient confidentiality.
Secure Documentation Practices
As we conclude our discussion on effective note-writing techniques, we must emphasise the importance of secure documentation and storage practices. These protocols are vital in safeguarding patient privacy and ensuring compliance with legal and regulatory standards.
1. Storing and Organizing Nursing Progress Notes
It’s essential to securely store nursing progress notes to protect patient information and comply with legal requirements. Use secure, encrypted storage solutions that meet privacy standards like HIPAA. Cloud-based systems are beneficial for ensuring easy access, compliance, and backup.
2. Benefits of Cloud-Based Solutions
Cloud-based platforms allow healthcare teams to:
- Access patient records 24/7.
- Comply with privacy regulations.
- Back up and recover data in case of an emergency.
These protocols are critical for safeguarding patient privacy and ensuring legal and regulatory compliance.
Protect patient privacy and simplify access with Practaluma’s secure, cloud-based storage. Switch today and benefit from the following services:
- Advanced Encryption to safeguard patient data from unauthorised access.
- Seamless, Role-Based Access Controls for efficient and secure information sharing.
- Compliance with Legal and Regulatory Standards to ensure patient confidentiality.
- Automated Backup and Recovery to prevent data loss and ensure business continuity.
- Intuitive User Interface for easy and efficient management of patient records.
Switch to Practaluma now and ensure your patient data is secure, accessible, and compliant.
Conclusion
Writing accurate, detailed, and timely nursing progress notes is vital for delivering high-quality aged care. These notes ensure continuity of care, improve communication across the healthcare team, and provide legal protection.
By following best practices, using structured templates, and documenting every aspect of patient care, you can enhance the quality of care and protect your patients and yourself.
Ready to Improve Your Documentation? Streamline your documentation with Practaluma's templates and tools. Start improving your nursing progress notes today!